Reducing Recurrence of Nonconformances with a Closed-Loop CAPA System
Learn how a closed-loop CAPA system helps reduce the recurrence of nonconformances in the medical device industry. Discover how digital solutions streamline corrective and preventive actions, enhance root cause analysis, and ensure continuous improvement, driving better product quality and compliance.

Addressing Persistent Quality Gaps with CAPA Software for Medical Device Industry
In the medical device sector, nonconformances are more than operational setbacksthey are critical threats to patient safety and business continuity. Reducing their recurrence requires not only swift detection but also systemic correction. CAPA Software for Medical Device Industry is designed to offer a strategic framework that identifies root causes and prevents recurrence through automated, traceable processes. An effective closed-loop corrective and preventive action (CAPA) system strengthens quality management and enables regulatory alignment across global markets.
A fragmented or manual CAPA process often leads to reactive responses rather than proactive quality improvements. By leveraging a digital CAPA software for medical device industry, manufacturers can ensure that every deviation, failure, or nonconformance is systematically captured, analyzed, and corrected within a unified quality management framework.
The Role of Closed-Loop CAPA in Sustaining Quality Management Excellence
Closed-loop CAPA ensures that quality issues are not only addressed but learned from. In a highly regulated environment, such as medical devices, traceability and accountability are non-negotiable. CAPA software provides full visibility into the issue lifecyclefrom detection through investigation to verification of effectivenessensuring that nothing falls through the cracks.
This continuous improvement cycle integrates with enterprise-wide quality management initiatives, bridging compliance with business performance. From internal audits to supplier management, CAPA processes tie into broader quality workflows, creating an interconnected system that proactively mitigates risks and reinforces patient safety.
Root Cause Analysis and Risk Prioritization in CAPA Software for Medical Device Industry
One of the central capabilities of CAPA software for medical device industry is root cause analysis. A reactive fix is not sufficient in a regulated domain where FDA inspections and ISO 13485 compliance demand evidence of systematic remediation. Whether the trigger is a complaint, audit finding, or nonconforming material report, CAPA systems prioritize high-risk issues and enable teams to analyze contributing factors with precision.
CAPA software supports tools such as the 5 Whys, fishbone diagrams, and failure mode effect analysis (FMEA), all within a standardized, validated environment. This allows teams to ensure consistency, reduce investigation time, and provide regulators with a detailed view of how potential risks are being managed effectively.
Integration with Quality Management for Comprehensive Compliance
The ability to integrate CAPA with quality management systems (QMS) is critical for holistic process control. When corrective and preventive actions are disconnected from broader quality processes, organizations lose critical context and traceability. CAPA software for medical device industry connects directly with quality event triggers such as complaints, audit findings, and out-of-spec results.
Such integration ensures that each CAPA is not an isolated task but a part of the broader quality ecosystem. Data from nonconformances, change control, and document revisions can automatically feed into CAPA workflows, enabling a single source of truth and ensuring that every decision is data-driven and audit-ready.
Enhancing Accountability and Cross-Functional Collaboration
CAPA requires input from multiple departments, from manufacturing and quality to regulatory and R&D. Without a centralized system, these collaborations can become chaotic, with inconsistent documentation, missed deadlines, or incomplete actions. CAPA software enforces accountability through assigned tasks, automated reminders, and escalations.
Workflows are standardized and transparent, allowing stakeholders to track status updates, monitor effectiveness checks, and share learnings across the enterprise. This transparency helps align teams toward a common goal: reducing the recurrence of Nonconformances and upholding a culture of quality.
Aligning CAPA Execution with FDA and ISO 13485 Requirements
Global compliance is a constant priority for medical device manufacturers. Regulatory bodies like the FDA and notified bodies in the EU assess the robustness of CAPA systems during audits and inspections. The FDAs Quality System Regulation (QSR) and ISO 13485 both emphasize the importance of an effective, well-documented CAPA process.
CAPA software for medical device industry automates documentation, captures decision rationales, and ensures that verification of effectiveness is complete before closure. This structured approach enables organizations to demonstrate full compliance and preparedness during regulatory assessments, reducing the risk of 483 observations or warning letters.
Leveraging Analytics for Continuous Improvement
One of the most powerful capabilities of digital CAPA software is the ability to leverage real-time analytics. Trends in recurring nonconformances, overdue actions, or ineffective CAPAs can be quickly identified and addressed. Dashboards provide executives with high-level summaries while enabling quality teams to drill down into granular data.
These insights are instrumental in refining quality management strategies and preempting risks. Organizations can benchmark performance over time, compare CAPA trends across sites, and allocate resources more effectively. This data-driven environment supports faster decision-making and strategic foresight in regulatory compliance.
Integrating Supplier-Related CAPAs for Extended Quality Oversight
Suppliers play a critical role in product quality and safety. A weak link in the supply chain can compromise the integrity of a device and lead to downstream failures. CAPA software for medical device industry includes tools to manage supplier-related nonconformances and initiate CAPAs collaboratively.
Suppliers can be assigned corrective tasks through controlled portals, with visibility into progress and effectiveness. This level of engagement reduces response time, improves traceability, and reinforces supply chain accountability. By embedding supplier performance into quality management systems, organizations strengthen their end-to-end compliance posture.
CAPA Closure and Effectiveness Verification
A CAPA is only as good as its resolution. Ensuring that the corrective or preventive action has indeed eliminated the root cause is critical for long-term quality assurance. CAPA software for medical device industry enforces a structured closure process, including documentation of implemented changes, follow-up audits, and effectiveness checks.
Effectiveness is not assumedit is demonstrated through evidence. Whether through testing, sampling, or audit outcomes, the closure process validates that the issue will not recur. This not only fulfills regulatory expectations but also builds confidence across stakeholders and customers.
Conclusion: Why ComplianceQuest is Essential for 2025 and Beyond
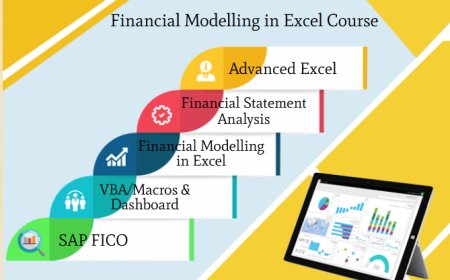
The future of medical device quality depends on intelligent, integrated solutions that streamline compliance, reduce risk, and drive operational excellence. ComplianceQuest offers a next-generation platform for managing CAPA within a broader QMS ecosystem. Built natively on the cloud and designed with flexibility, scalability, and global compliance in mind, it supports manufacturers in their pursuit of product and process integrity.
From root cause investigation to real-time analytics and supplier engagement, ComplianceQuest empowers quality leaders with tools that go beyond regulatory checkboxes. By adopting a closed-loop CAPA strategy supported by ComplianceQuest, companies in the medical device industry can reduce the recurrence of nonconformances, enhance their audit readiness, and maintain a strong commitment to patient safety in 2025 and the years to follow.